Overview
A 35-year-old lady presented with severe left sided radicular leg pain to A & E. She was highly distressed, and had a significant psychosocial history presenting with multiple yellow flags. She underwent an urgent MRI scan of the lumbar spine which showed a significant disc prolapse at L5/S1. As she was also reporting issues with bladder control, saddle anaesthesia and had both objective and subjective weakness in the S1 myotome, she went on to have an urgent discectomy. Following surgery, she continued to report high levels of distress and pain, but was discharged home nonetheless. She was reviewed in the spinal outpatient’s department four weeks later and still reported ongoing symptoms, at which point in time the spinal surgeon referred her for an urgent pain clinic review.
The lady presented to the pain clinic as a new patient at around 8 weeks following surgery. She presented in a highly distressed fashion, reporting severe pain affecting her back and both legs the left worse than the right. She was unable to sit and requested to lay down on the examination couch when she entered the clinic room. She reported that she felt she was worse rather than better since having had surgery. She could still pass urine unaided but reported urgency of micturition with hesitancy when it came to passing urine. She also continued to report saddle numbness. On examination, the surgical scar appeared well healed, but she was exquisitely tender around it and it was very difficult to make any meaningful neurological examination due to high levels of distress and reported pain.
By this point in time, she was taking Gabapentin 600mg tds, Amitriptyline 20mg nocte, Oramorph 10mg being taken four to five times per day, Diazepam 5mg tds as well as Co-Codamol 30/500mg two tablets four times daily. She rated her pain as 10 out of 10 on a Verbal Rating Scale and scored very highly on a Pain Self Efficacy Score and Oswestry Disability Index.
- How would you manage this patient?
- What are the potential differential diagnoses?
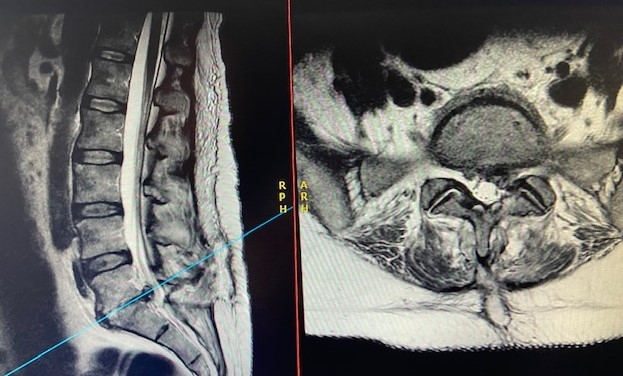
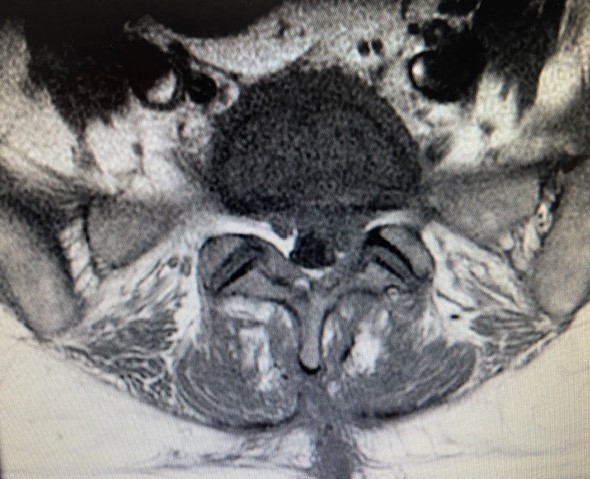
The patient was referred for an urgent Full blood count, ESR and CRP – results obtained later that day showed a white cell count of 14,000 x 109 per Litre, ESR of 120, and CRP of 180. On the basis of these results, she was recalled urgently the same day and underwent an urgent MRI scan which showed these images:


Diagnosis & Discussion
The patient was diagnosed with Discitis associated with recurrent disc prolapse, epidural abscess.
Discitis is an uncommon condition that involves infection of any of one or more of the intervertebral discs. Although it can happen spontaneously, it can also occur after surgery as in this case or after injections around the spine. A high index of suspicion is required in particular when patients have a background of severe uncontrolled pain or have had a previous intervention. A raised white cell count, ESR and CRP are strong indicators of an underlying infection and warrant urgent MRI. A stir sequence can also provide useful information when the radiological imaging is not as clear. In this reported case, there is clear evidence of an underlying inflammatory process as well as a recurrent disc prolapse.
Consider looking at the following suggested reading to learn further about discitis and its management.
Suggested Reading
- National Library of Medicine: Diskitis - Joseph D. Muscara; Eric Blazar. https://www.ncbi.nlm.nih.gov/books/NBK541047/
- The diagnosis and management of discitis and spinal infection - David A. Samy, Surya Gandham, Marcus DeMatas Surgery (Oxford) Volume 39, Issue 8, August 2021, pages 540-546 https://www.sciencedirect.com/science/article/abs/pii/S0263931921001423
- Non-infectious thoracic discitis: A diagnostic and management dilemma. A report of two cases with review of the literature Clinical Neurology and Neurosurgery. Volume 190, March 2020, 105648 https://www.sciencedirect.com/science/article/abs/pii/S0303846719304445
- Spondylodiscitis—a cohort analysis of its identification and management Farzan Dholoo, Anjali Sriramanarayanan, Savi Prabha Krishna Prasad, James Livingstone, Nicki Lewis, Vishal Prasad, Ashwin Unnithan International Orthopaedics Volume 47, pages 813–818 (2023)
https://link.springer.com/article/10.1007/s00264-022-05662-0
